The clinical foundation of the Reza Band is built upon a comprehensive, prospective, multicenter study designed to validate the safety and effectiveness of external Upper Esophageal Sphincter (UES) compression. This landmark research addressed a critical gap in the treatment of Laryngopharyngeal Reflux (LPR), focusing on patients whose symptoms persisted despite standard-of-care medical interventions. By utilizing a mechanical approach to treat a mechanical dysfunction, the study provided definitive proof that external reinforcement of the UES can effectively stop the backflow of gastric contents into the throat.

Study Objective And Systematic Methodology
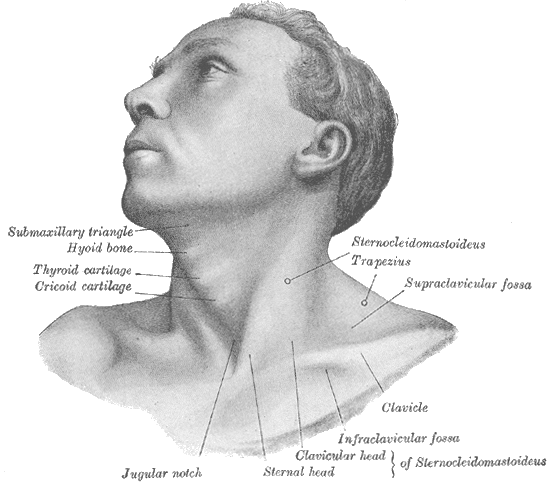
The primary objective of the clinical evaluation was to quantify the impact of targeted cricoid pressure on the frequency and severity of LPR symptoms. Investigators sought to determine if a non-invasive, wearable device could provide a sufficient mechanical barrier to replace or augment traditional pharmacological therapies.
- Diverse Patient Enrollment: The study recruited subjects from multiple leading ENT and gastroenterology clinics, ensuring a broad demographic and clinical representation.
- Inclusion Criteria: Participants were required to have a confirmed diagnosis of LPR and a high baseline Reflux Symptom Index (RSI) score, indicating moderate to severe daily impairment.
- The Intervention Protocol: Upon enrollment, each patient was professionally fitted with a Reza Band calibrated to apply 20-30 mmHg of pressure specifically to the cricoid cartilage area.
- Data Collection Milestones: Subjective symptom changes and objective safety data were recorded over a multi-week trial, with primary endpoints measured at the two-week and four-week intervals.
Quantitative Success Metrics: Symptom Resolution
The data gathered during the multicenter study revealed a statistically significant improvement in nearly all clinical markers of LPR. The findings established the Reza Band as a highly effective tool for rapid symptom management.
- The 86% Efficacy Benchmark: A total of 86% of study participants were classified as "treatment successes," meaning they achieved a clinically significant reduction in their overall symptom burden.
- Drastic RSI Score Reduction: The mean Reflux Symptom Index (RSI) scores—the gold standard for measuring LPR—dropped from a baseline of 25.6 to 14.6 within the first 14 days of nightly use.
- Relief from Chronic Airway Irritation: Patients reported a marked decrease in the most debilitating "silent reflux" symptoms, including chronic coughing, hoarseness, and persistent throat clearing.
- Resolution of Globus Sensation: The uncomfortable feeling of a "lump" in the throat, a hallmark of UES dysfunction, showed significant resolution across the study cohort.
- Long-Term Consistency: Case reviews associated with the study showed that patients like Ted Mueller experienced total resolution of chronic reflux symptoms within 30 days of beginning therapy.
Professional Validation And Patient Compliance
Beyond symptom reduction, the study evaluated the practical application of the device within a real-world medical environment, focusing on physician confidence and patient ease of use.
- Broad Physician Acceptance: 92% of the medical professionals overseeing the clinical trials reported they were satisfied or very satisfied with the device’s clinical performance.
- A Validated Alternative to PPIs: Prescribing physicians noted that the device provided a necessary solution for "non-responders" who saw little to no improvement from traditional acid-suppression drugs.
- High Patient Satisfaction: Approximately 75% of patients expressed high satisfaction with the treatment, often citing the relief of nightly symptoms that had previously disrupted their sleep.
- Nightly Use Feasibility: Despite being a neck-worn device, participants found the band to be tolerable for long-term nocturnal use, with many reporting they felt "more in control" of their health journey.
Rigorous Safety Profile Analysis
A paramount goal of the multicenter evaluation was to ensure that applying external pressure to the neck did not result in unintended side effects or safety concerns.
- Zero Serious Adverse Events: Throughout the entire duration of the multi-center clinical evaluation, there were no reports of serious or unexpected adverse events.
- Non-Invasive Advantage: By operating externally, the Reza Band avoided the surgical complications and systemic side effects typically associated with long-term pharmacological or operative interventions.
- Mechanical Safety: The device was found to be a safe, drug-free option for managing the physical backflow of acid, pepsin, and bile into the respiratory tract
Conclusion Of The Multicenter Trial
The results of this clinical study provided the necessary evidence to establish the Reza Band as a primary therapeutic option for LPR. By demonstrating an 86% success rate and an impeccable safety record, the research confirmed that mechanical UES reinforcement is an effective, non-surgical, and drug-free way to restore the body’s natural defense against reflux. The study underscores the importance of medical supervision, as professional fitting remains the key to achieving these validated clinical outcomes.


.svg)
